This resource was updated by a member of The Open Sanctuary Project’s staff on January 17, 2025.

Veterinary Review Initiative
This resource has been reviewed for accuracy and clarity by a qualified Doctor of Veterinary Medicine with farmed animal sanctuaryAn animal sanctuary that primarily cares for rescued animals that were farmed by humans. experience as of April 2022.
Check out more information on our Veterinary Review Initiative here!
HPAI Has Now Been Detected In Mammalian Farmed AnimalA species or specific breed of animal that is raised by humans for the use of their bodies or what comes from their bodies. Species As Well
On March 20, 2024, The Minnesota Board Of Animal Health (MBAH) announced the first detection of highly pathogenic avian influenza (HPAI) in a domesticated ruminant in the U.S. after a goat kidA young goat in Stevens County tested positive. Soon after, HPAI was detected in cowsWhile "cows" can be defined to refer exclusively to female cattle, at The Open Sanctuary Project we refer to domesticated cattle of all ages and sexes as "cows." at dairies in Texas and Kansas and has since been detected in hundreds of cows across numerous states. Alpacas and pigs have also been affected. This is a developing situation. For more information about HPAI in mammalian farmed animal species and an overview of states affected, check out our resource here.
Please note that we have updated this resource slightly to reflect the new and evolving information about detections in mammalian farmed animalsA species or specific breed of animal that is raised by humans for the use of their bodies or what comes from their bodies. species and how this impacts or may impact birds. This textbox, as well as the “Updated” textboxes, were added to reflect the current situation and, unlike the rest of the information in this resource, have not yet been reviewed by a veterinarian.
-On October 21, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Newport County, Rhode Island.
-On October 7, 2022, the USDA confirmed the presence of HPAI in commercial broiler breeder chicken flock in Madison County, Arkansas.
-On October 6, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Bernalillo County, New Mexico.
-On September 15, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Obion County, Tennessee.
-On August 10, 2022 the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Sacramento, California.
-On July 22, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Seminole County, Florida.
-On July 18, 2022 the USDA confirmed the presence of HPAI in a non-commercial, backyard flock in Carson City, Nevada.
-On June 2, 2022 the USDA confirmed the presence of HPAI in a non-commercial, backyard flock in Toombs County, Georgia.
-On May 18, 2022, the USDA confirmed the presence of HPAI in in a non-commercial backyard flock in Monmouth County, New Jersey.
-On May 6, 2022, the USDA confirmed the presence of HPAI in a non-commercial, backyard flock in Linn County, Oregon and a non-commercial backyard flock in Pacific County, Washington.
-On May 1, 2022, the USDA confirmed the presence of HPAI in a commercial chicken flock in Sequoyah County, Oklahoma.
– On April 30, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Matanuska-Susitna Borough, Alaska.
-On April 29, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Caledonia County, Vermont.
-On April 16, 2022, the USDA confirmed the presence of HPAI in a commercial chicken flock in Lancaster County, Pennsylvania, and a non-commercial backyard flock in Utah County, Utah.
-On April 15, 2022, the USDA confirmed the presence of HPAI in two flocks in Idaho – a non-commercial, backyard flock in Caribou County and a non-commercial, backyard flock in Gooding County.
-On April 9, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Pitkin County, Colorado.
-On April 8, 2022, the USDA confirmed the presence of HPAI in in two flocks in Montana – a non-commercial, backyard flock in Cascade County, and a non-commercial, backyard flock in Judith Basin County.
-On April 2, 2022, the USDA confirmed the presence of HPAI in a commercial pheasant flock in Erath County, Texas.
-On March 30, 2022, the USDA confirmed the presence of HPAI in a non-commercial, mixed-species backyard flock in Berkshire County, Massachusetts; a non-commercial, mixed-species backyard flock in Johnson County, Wyoming; a commercial poultry flock in Johnston County, North Carolina; a non-commercial, backyard chicken flock in Franklin County, Ohio; and a non-commercial, backyard chicken flock in Kidder County, North Dakota.
-On March 26, 2022 the USDA confirmed the presence of HPAI in in two flocks in Minnesota – a commercial turkey flock in Meeker County and a backyard mixed species flock in Mower County.
-On March 17, 2022, the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Rockingham County, New Hampshire.
-On March 16, 2022 the USDA confirmed the presence of HPAI in a non-commercial backyard flock in Merrick County, Nebraska.
-On March 14, 2022, the USDAThe United States Department of Agriculture, a government department that oversees agriculture and farmed animals. confirmed the presence of HPAI in a commercial layer chicken flock in Jefferson County, Wisconsin.
– On March 12, 2022, the USDA confirmed the presence of HPAI in a backyard mixed species poultry flock in Franklin County, Kansas and a backyard flock in McLean County, Illinois.
– On March 6, 2022 the USDA reported confirmed cases of HPAI in a commercial mixed species flock in Charles Mix County, South Dakota.
– On March 5, 2022 the USDA reported confirmed cases of HPAI in a commercial chicken flock in Cecil County, Maryland.
– On March 4, 2022 the USDA reported confirmed cases of HPAI in a commercial chicken flock in Stoddard County, Missouri.
– On March 2, 2022 the USDA reported confirmed cases of HPAI in two non-commercial backyard flocks in Connecticut and Iowa
– On February 24, 2022 the USDA reported confirmed cases of HPAI in a backyard flock in Kalamazoo County, Michigan
– On February 23, 2022 the USDA reported confirmed cases of HPAI in a commercial chicken flock in New Castle County, Delaware.
– On February 20, 2022, the USDA reported confirmed cases of HPAI in a non-commercial backyard flock in Knox County, Maine.
– On February 19, 2022 the USDA reported confirmed cases of HPAI in a non-commercial backyard flock in Suffolk County, New York.
– On February 14, 2022, the USDA reported confirmed cases of HPAI in a commercial chicken flock in Fulton County, Kentucky and also in a backyard flock in Fauquier County, Virginia
– On February 9, 2022, the USDA reported confirmed cases of HPAI in domesticated turkeys in Dubois County, Indiana
-On November 15, 2024, the USDA reported confirmed cases of HPAI in a backyard flock in Central Oʻahu.
-On December 18, 2024, California proclaimed a State of Emergency to streamline and expedite the state’s response to HPAI.
-On January 13, 2025, The USDA announced the detection of HPAI in a backyard poultry flock in Puerto Rico.
Update April 10th, 2024 – This Resource Is Focused On Avian Influenza In Birds
Please note that this resource was written before HPAI had been detected in mammalian farmed animal species. The guidance and information contained within were written specifically with domesticated birds, and more specifically, farmed bird species, in mind. While some of this information is important to understand when thinking about HPAI in mammalian species, please know that not all of the information in this resource can be applied to mammals. For example, clinical signs, necessary biosecurityMerck Veterinary Manual defines biosecurity as ”the implementation of measures that reduce the risk of the introduction and spread of disease agents [pathogens].” measures, and the implications of a positive test can be quite different for birds than for mammalian residents. For specific information about HPAI in mammalian farmed animal species, please check out our FAQ here.
Update September 16, 2024 – HPAI Detections In Humans
Infections of avian influenza in humans have been detected in countries worldwide. For a report from the World Health Organization, as well as regularly updated “situation reports,” you can check out this page. For updates specific to the United States, you can check out the Center For Disease Control’s Avian Influenza page here.
RESOURCE GOALS:
- Understanding the basics about the various viruses that cause “avian influenza”;
- Learning about the common vectors of avian influenza infection;
- Identifying biosecurity measures that can be taken at your sanctuary to minimize risk to both your residents and their caretakers;
- Being able to identify common signs of avian influenza infection in residents and knowing what steps to take;
- Developing an understanding of what a positive test for avian influenza may or may not mean;
- And learning what measures you can take from a sanctuary administrative perspective to safeguard your residents.
Stay Tuned For Updates
As of this writing, there are HPAI outbreaks globally, including in the US. As the situation develops, we’ll update this resource with new information and guidance as we receive it.
Frequently Asked Questions And Checklist
While we encourage folks to read through this resource, if you’re looking for an introductory guide, you can start by checking out our Avian Influenza FAQ here. If you’re looking for an actionable checklist to start implementing strategies to protect your residents, check out our HPAI checklist here.
What Is Avian Influenza (AI)?
The term “avian influenza” refers to any disease or infection in birds that is caused by Type A influenza viruses. These viruses are divided into subtypes based on two proteins on the surface of the virus- hemagglutinin (HA) and neuraminidase (NA). There are 16 HA subtypes (H1-H16) and 9 NA subtypes (N1-N9). These HA and NA subtypes form many different combinations (i.e H9N2, H5N1, H7N2, etc.). Most subtype combinations have been reported in domesticated or wild birds though their distribution varies.
Free-flying aquatic birds (such as migratory waterfowl and shorebirds) are the natural host of Type A influenza viruses, but these viruses can also affect domesticated farmed birds (including chickens, turkeysUnless explicitly mentioned, we are referring to domesticated turkey breeds, not wild turkeys, who may have unique needs not covered by this resource., pheasants, quail, ducksUnless explicitly mentioned, we are referring to domesticated duck breeds, not wild ducks, who may have unique needs not covered by this resource., and geeseUnless explicitly mentioned, we are referring to domesticated goose breeds, not wild geese, who may have unique needs not covered by this resource.) as well as other bird species. Human infections have occurred, but these are rare and usually involve H5 or H7 strains. In addition to humans, Type A influenza viruses have also been isolated from other mammalian species including mice, rats, weasels, ferrets, cats, dogs, pigs, and horses.
Virus strains are categorized as highly pathogenic avian influenza (HPAI) viruses or low pathogenic avian influenza (LPAI) viruses. HPAI viruses develop as a result of mutations of some H5 and H7 LPAI viruses and are extremely dangerous for chickens, turkeys, and related species. In chickens, turkeys, and other GalliformesOrder of heavy-bodied ground birds including chickens, turkeys, guinea fowl, quail, and peafowl, HPAI causes severe systemic disease and can result in widespread organ failure and sudden death. HPAI carries a high mortality rate which may reach 100% within a few days. LPAI, on the other hand, typically has a low morbidity and mortality rate and with outcomes ranging from asymptomatic infections to more serious respiratory illness.
Thankfully, most Type A influenza viruses are low pathogenic. LPAI viruses are found worldwide and are frequently found in apparently healthy migrating waterfowl and shorebirds. These species rarely develop clinical disease from infection unless H5N1 HPAI is involved. H5 HPAI viruses of Eurasian lineage have caused mortality in both wild and domesticated waterfowl as well as other bird species. (Highly pathogenic Eurasian H5 avian influenza was detected in South Carolina and North Carolina in mid-January 2022 after not being detected in a wild bird in the US since 2016.)
How Is AI Spread?
Infected birds shed AI virus from their nareseither of the pair of openings of the nose or nasal cavity, mouth, conjunctiva, and cloaca. Additionally, HPAI viruses have been found in the feathers, feather follicles, and preen glanda large gland that occurs in most birds, opens dorsally at the base of the tail feathers, and usually secretes an oily fluid which the bird uses in preening their feathers (also known as an oil gland or uropygial gland) of infected individuals. Spread via respiratory secretions and feces play a major role in transmission. Susceptible birds can become infected via inhalation or ingestion of the virus resulting from direct contact with infected birds (including wild birds) or via indirect contact through aerosol droplets or contaminated fomitesObjects or materials that may become contaminated with an infectious agent and contribute to disease spread.
Avian influenza is highly contagious and spreads easily within the same species and can also spread between closely related host species within the same taxonomic family (such as between chickens, turkeys, partridges, and quail- all belonging to the family Phasianidae). Transmission between species belonging to different taxonomic orders within the same class is also possible (such as from duckUnless explicitly mentioned, we are referring to domesticated duck breeds, not wild ducks, who may have unique needs not covered by this resource. to turkeyUnless explicitly mentioned, we are referring to domesticated turkey breeds, not wild turkeys, who may have unique needs not covered by this resource.) but occurs less often than between more closely related species. Transmission between different classes occurs even less frequently, such as between chickens and humans. According to David E. Swayne, David L. Suarez, and Leslie D. Sims, in Diseases of Poultry 13th Edition, “One exception to the preceding rule has been the ease and frequency of transfer of swine H1N1 and H3N2 viruses to turkeys when the two species were raised in close geographic proximity.” They go on to explain that many factors affect the virus’ ability to spread within or between species. These factors include the intermixing of species, the age and population density of birds, as well as the weather and temperature.
In terms of the possible ways in which AI viruses can be introduced to a flock, Swayne, Suarez, and Sims highlight four possible sources (though the risk associated with each varies depending on how likely it is that these sources will come into contact- direct or indirect- with susceptible birds). While their focus is on virus introduction to commercial settings, it’s helpful to consider these sources of infection and the role they might play in sanctuary settings. They list these initial sources of infection as including:
- Other domesticated “poultry”
- Migratory waterfowl and other wild birds
- Domesticated pigs
- “PetAn animal who spends regular time with humans in their home and life for companionship or human pleasure. Typically a small subset of animal species are considered to be pets by the general public.” birds
How Does AI Manifest?
There are many factors that impact how AI manifests. These factors include whether or not the virus is highly pathogenic (HPAI) or low pathogenic (LPAI), as well as environmental factors and factors specific to the individual(s) such as their species, age, sex, health, and whether or not they have acquired immunity.
Swayne, Suarez, and Sims categorize AI into four clinical groups based on mortality patterns, lesions, and clinical signs. These clinical groups are highly virulent, moderately virulent, mildly virulent, and avirulent and are described as follows:
- Highly Virulent– This clinical group is the result of infection with HPAI H5 or H7 viruses, usually in chickens or other closely related species. Disease is severe, highly fatal (with morbidity and mortality nearing 100%), and systemic (with most organ systems affected).
- Moderately Virulent– This clinical group is the result of LPAI viruses, usually accompanied by co-infection or other stress factors. Mortality rates are highly variable, ranging from 5% to 97% with the highest mortality rates occurring in actively laying hens, young birds, and birds who are severely stressed.
- Mildly Virulent– This clinical group is the result of LPAI viruses resulting in mild respiratory disease and reduced egg laying in females. Mortality is low (typically below 5%) and most often seen in older birds.
- Avirulent– This clinical group is also the result of LPAI viruses but does not cause any clinical signs or increased mortality. Avirulent AI is most often seen in wild waterfowl and shorebirds infected by LPAI viruses.
What Are The Clinical Signs Of AI?
As mentioned above, there are many factors that impact how AI manifests, but whether or not the virus is HPAI or LPAI plays a major role. (As a side note, most of the available information on avian influenza in domesticated birds focuses on chickens and turkeys. Comparatively, there is less information about domesticated ducks and even less specifically regarding geese.)
Clinical Signs of HPAI In Chickens, Turkeys, And Related Gallinaceous Species
Clinical signs of disease in chickens, turkeys, and related species vary depending on which specific organs and tissues are affected and the extent of damage done. Therefore, not all clinical signs will present in every individual. Due to the sudden onset, in chickens and turkeys, it is not uncommon for the first sign of HPAI to be the death of multiple birds. Clinical signs of HPAI in chickens, turkeys, and related gallinaceousBelonging to the order Galliformes (heavy-bodied ground birds, including chickens, turkeys, guinea fowl, quail, and peafowl) species include:
- Neurological signs such as tremors of the head and neck
- Inability to stand
- Unusual positioning of the head or extremities (such as arching the head backward or twisting of the neck)
- Loss of appetite
- Listlessness
- In actively laying hens, a sudden drop in egg production
- Cyanosis and edemaEdema is the abnormal accumulation of fluid in tissues of the body. of the head, comba fleshy crest on the head of the domestic chicken and other domesticated birds, wattlea fleshy pendulous process usually about the head or neck (as of a bird), and snood
- Edema and reddening of the legs and feet
- NecrosisNecrosis is the death of most or all of the cells in an organ or tissue due to disease, injury, or failure of the blood supply. and hemorrhage of the non-feathered skin
- Blood-tinged discharge from the eyes and nares
- Sneezing, coughing, and abnormal breathing sounds
- Green diarrhea
- Sudden death
Clinical Signs Of HPAI In Waterfowl
Most HPAI viruses are poorly adapted to non-gallinaceous species and, therefore, replicate within them only to a limited degree. Mortality rates from HPAI in domesticated ducks and geese have been low, and both domesticated and wild waterfowl often show few clinical signs. However, highly pathogenic H5N1 is the exception and can cause clinical disease in waterfowl with signs including:
- Depression
- Loss of appetite
- Neurological signs
- Sudden death
- Corneal opacity (noted in domesticated ducks)
Clinical Signs Of LPAI
As explained earlier, LPAI can manifest in various ways depending on factors such as the age and species of the individual and whether or not there are co-infections or other stressors. Clinical signs may be related to infection of the respiratory, reproductive, digestive, or urinary tract, but respiratory illness is most common. Clinical signs of LPAI may include:
- Mild to severe respiratory signs such as:
- Sneezing and “coughing”
- Abnormal breathing sounds
- Discharge from the eyes and nares
- Swelling of the infraorbital sinuses (sinusitis is common in turkeys, quail, and ducks)
- Reproductive signs in females, such as:
- Misshapen, fragile eggs
- Increased broodiness
- Decreased egg laying in actively laying hens
- Ruffled feathers
- Lethargy
- Decreased appetite
Is There Any Treatment For AI?
Unfortunately, there is no specific treatment for AI, but depending on the strain and manifestation, supportive care and treatment of secondary infections may be necessary. If you suspect one of your residents may have AI, isolate them immediately and consult with your veterinarian with respect to treatment. Keep in mind that veterinarians are subject to reporting requirements with respect to testing – even suspected cases may have implications for the individual and their flockmates. In this kind of situation, it is critical to have a good isolationIn medical and health-related circumstances, isolation represents the act or policy of separating an individual with a contagious health condition from other residents in order to prevent the spread of disease. In non-medical circumstances, isolation represents the act of preventing an individual from being near their companions due to forced separation. Forcibly isolating an individual to live alone and apart from their companions can result in boredom, loneliness, anxiety, and distress. protocol in place and a good relationship with your veterinarian in order to ensure the well-being of the resident in question, as well as the safety of the rest of your flock.
While prevention of disease, rather than trying to treat disease, is always the best option, when it comes to HPAI, prevention is the only way to ensure the well-being of your residents. Not only does HPAI put your residents in grave danger due to the disease’s high mortality rate, regional efforts to control disease spread also put your residents at risk. (We’ll talk more about how to protect residents from HPAI below).
What If One Of My Residents Tests Positive For AI?
Before we attempt to answer this question, it’s important to consider that there are multiple reasons a bird might be tested for AI in the first place. AI screening tests are often part of transport requirements when traveling from one state or region to another. A positive result in this case might be treated very differently than a positive test in a bird who is showing clinical signs of illness or a positive test during an HPAI outbreak. If you are considering rescuing birds from out of state, adopting residents to homes out of state, or using screening testing for another reason, we recommend having a conversation with your veterinarian about what would happen if a resident were to test positive for AI, so you can fully understand the risks involved.
Screening tests for AI test for Type A influenza virus. In the event of a positive result, further diagnostics would be necessary to determine the subtype. In the US, each state has their own initial response plan in place to confirm or rule out low pathogenic H5 and H7 AI (which, again, are of greater concern than other LPAI subtypes due to their ability to mutate into HPAI). In the event that one of your residents tests positive for AI on a screening test but are not showing signs of illness, it may be helpful to consider these words from Dr. Dale Lauer of the Minnesota Board Of Animal Health- “Generally, if you don’t see clinical disease, the odds are it’s probably low path AI. However, clinical disease could be either high path or low path.”
How Can I Protect My Residents From AI?
While the idea of your residents becoming infected with a potentially serious disease is concerning enough, some of the biggest fears that come with the thought of AI is what will happen to residents if there is an HPAI outbreak nearby (as one mitigation measure often employed is the killing of birds who have been infected with or exposed to HPAI viruses) and what will happen to residents if just one individual tests positive for AI, even if they aren’t showing any clinical signs.
When considering how to protect your residents from the viruses that cause avian influenza, it’s first important to consider the current level of risk. During low-risk times, measures such as robust quarantineThe policy or space in which an individual is separately housed away from others as a preventative measure to protect other residents from potentially contagious health conditions, such as in the case of new residents or residents who may have been exposed to certain diseases. procedures for incoming residents and practicing good biosecurity will help protect your residents from various infectious diseases. However, during high-risk times (such as when HPAI has been confirmed in nearby regions or when experts are predicting cases or are raising the alarm over high numbers of low pathogenic H5 or H7), enhanced biosecurity measures will be necessary. In the webinar, Defending The Flock: Preventing Avian Influenza Introductions: Focus On The Big Risks, Dr. Carol Cardon explains that the increased levels of virus particles in the environment when HPAI has been detected means we need more effective measures to eliminate those viruses, and we also need increased precision. She uses the following examples: during “normal” times, consider that there might be 100 virus particles on a caregiverSomeone who provides daily care, specifically for animal residents at an animal sanctuary, shelter, or rescue.. Biosecurity measures that are 99% effective will result in one particle making it into resident living spaces, which is not enough to infect a bird. However, if there are 100 billion virus particles in the environment, those same biosecurity measures would still allow for one billion particles to make it into resident living spaces.
Therefore, in addition to having quarantine and general biosecurity protocols in place, one of the most important ways to protect your residents from AI is to stay up-to-date about the current situation and potential risk of HPAI both in your area and more broadly. Because the virus is spread by migratory birds, outbreaks in other parts of the world could increase the level of concern in your area, even if you are separated by thousands of miles of ocean. We recommend you check in with your veterinarian or local officials regarding where to find the most up-to-date information for your area. For folks in the US, the USDA announces the first confirmed case of HPAI in domesticated birds in each state and maintains a list of each confirmed case in both domesticated and wild birds. Additionally, you can refer to The Organisation For World Animal Health (OIE) Situation Reports on Avian Influenza.
During periods of confirmed cases of HPAI, it’s a good idea to have a designated person in charge of monitoring cases in your state and surrounding counties and having them relay that information to those involved in decision making and animal care. This way, your organization can stay up to date and make changes to your protocols if the degree of risk in your area changes.
How Can I Protect My Residents During Times Of High Risk?
Please Defer To Your Veterinarian Or Local Government Officials!
Below we’ll discuss some of the measures that can help mitigate introduction of the virus to your residents during times when there is high risk of HPAI. However, different regions will have different rules, regulations, and guidelines. You must be aware of these and make sure you are following any requirements they have put in place (including necessary recordkeeping). Your veterinarian or regional governing body will be the best source of this information.
During times of high risk, the degree of risk in different areas will vary, and the risk to your area can change quickly, so be sure to work with your veterinarian or regional officials to determine the degree of risk in your area and to determine what protective measures are most appropriate. We recommend that all farmed bird caregivers have plans in place to protect residents so that they can implement appropriate protective measures quickly if and when the degree of risk changes in their area.
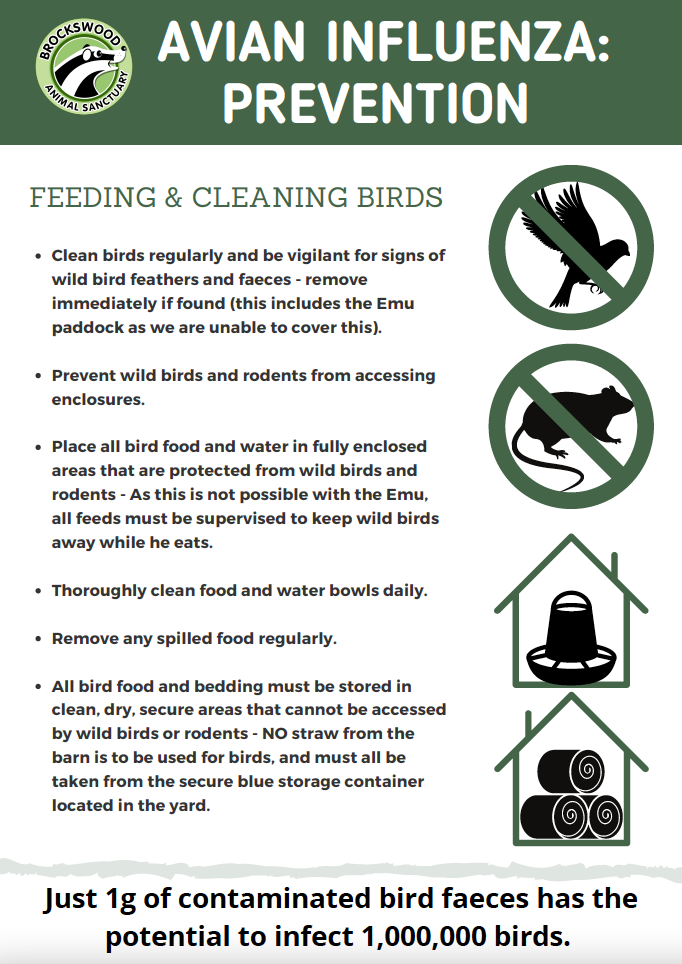
Prevent Contact With Wild Birds (Both Direct and Indirect)
Because wild birds can introduce avian influenza viruses to your property and residents, taking steps to prevent direct and indirect contact between residents and wild birds is an important way to protect your residents. This includes:
Keep Bird Residents In Enclosed Spaces
Enclosing bird resident living spaces will prevent wild birds, as well as their feces and feathers, from coming into contact with residents. This may be accomplished by covering their outdoor spaces with a solid roof and covering the sides with window screen or mesh/netting with openings that are small enough to prevent wild birds and rodents from entering the space. In order to continue to give residents access to natural light, some caregivers have opted for clear roofing materials. Due to their relative ease of installation, others have employed heavy-duty tarps. Whatever material is chosen, in areas with snow, be sure to factor in that these materials may not be able to sustain the weight of snow, which could result in a dangerous collapse. If outdoor spaces cannot be covered, residents should be kept indoors. If neither of these options are possible, and there is not a direct order to keep birds under a solid roof, you could consider using screen, mesh, or netting to prevent wild birds from entering the space. This will not ensure that all possible sources of infection, such as feces or feathers, do not come in contact with residents (especially if the space is under trees or other spaces where wild birds congregate), but can potentially help reduce spread, especially if other precautions are taken. Again, defer to your veterinarian and governing agency.
After taking steps to enclose your residents’ living spaceThe indoor or outdoor area where an animal resident lives, eats, and rests., be sure to regularly monitor enclosures to ensure materials are holding in place and there are no breaches, and take immediate steps to fortify when needed. If the risk in your area is not currently high, but there is concern HPAI could spread to your area, we urge you to start making plans now for how you would cover outdoor spaces or otherwise keep wild birds (and their feces and feathers) away from your residents and their living spaces.


Protect Resident Food And Water
If you are unable to cover your residents’ outdoor space with a solid roof but can use screen, mesh, or netting, you absolutely must ensure food and water sources are protected from wild birds and their feces, which may be accomplished by keeping food and water under cover at all times. Without measures to keep wild birds out of bird resident living areas, simply putting food and water underneath an overhang or solid table will not be enough as wild birds will be able to fly under the cover and get directly to the food and water. However, in enclosures with a barrier that keeps wild birds out but has openings that could allow feces, feathers, or other sources of infection to enter the space, keeping food and water sources covered will help protect them from becoming contaminated.
Store Food And Bedding Securely
In addition to keeping resident spaces and the food and water they have access to protected from wild birds and rodents, ensure food and bedding reserves are stored in secure areas where wild birds and other wildlife cannot access them. For example, if you use straw, keeping straw bales in a storage building that wild birds can access means bedding could become contaminated and, once brought into bird resident living spaces, could expose residents to these viruses. Food stores should be kept in solid containers that keep wild birds and other wildlife out. Be sure to inspect bedding and food storage areas to ensure there has not been a breach, and do not use supplies that could have been contaminated.
Keep Tools And Supplies Protected
Contaminated tools and supplies can act as fomites, exposing your residents to avian influenza viruses. To prevent this from happening, be sure to store tools (such as those used for cleaning) and other supplies that are used with or brought into bird resident living spaces in a secure area where wild birds cannot contaminate them. Ideally, each bird resident group should have their own designated tools that are stored within the living space to prevent contamination. Any crates or carriers used to house or transport birds should be thoroughly cleaned and disinfected both before and after use.
Disinfectants
When choosing a disinfectant, be sure to choose one that is effective against avian influenza, as well as appropriate for your intended use. You can find more information about disinfectants registered for use against avian influenza at the EPA’s website here (as well as a link to a list of disinfectants). You can also read more about disinfectants and HPAI in Chapter 11 of this manual from The Food and Agriculture Organization of The United Nations. We recommend talking with your veterinarian about which disinfectant products to use, making sure you know what, if any, risks they pose to your residents and how those risks can be minimized or avoided.
Keep Waterfowl Residents Separated From Other Bird Residents
Because waterfowl are especially susceptible to Type A influenza viruses, and because they can be infected without showing clinical signs, most recommendations include keeping domesticated waterfowl completely separate from other farmed birds. Do not allow them to have access to ponds wild waterfowl also have access to (or that are fed by a water source that could be contaminated).
Update November 7, 2024 – Keep Avian Residents Separate From Mammalian Residents
In general, we think it’s best to house avian residents separate from mammalian residents, but given the current situation with HPAI detections in mammalian farmed animal species, this is imperative. Evidence suggests the virus can be spread between cows and farmed birds (including via indirect contact). Additionally, several cases in mammalian farmed animals have occured in situations where they shared space and drinking water with farmed bird species.
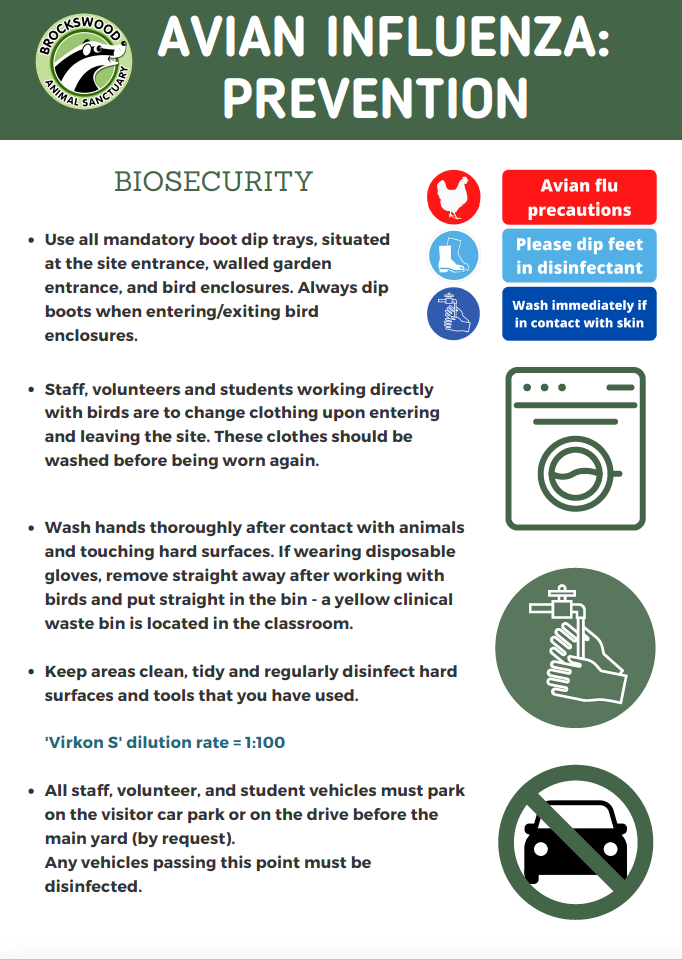
Mitigate The Risk Of Spread Due To Human Movement
Wild birds are not the only way the virus can be introduced to your property. Humans who have come into contact with the virus can carry it on their clothes, shoes, hands, etc., and vehicles and equipment that have come into contact with AI viruses can also be a source of introduction to your property. Measures that can help reduce the risk of virus spread associated with human movement include the following:
Limit The Number Of Humans Coming Onto Your Property
If the risk of HPAI is high, you really want to keep the number of humans (and their vehicles) coming onto your property to a minimum. If you have a visitor program and have not already been instructed by government officials to put it on hold, you should strongly consider temporarily suspending the program and related onsite activities.
Create A Controlled Access Point
If you can, have vehicles park right at or near the entry to your property so as to mitigate the risk of vehicles bringing the viruses further onto your property. Having a controlled access point with clear signage and a physical barrier also ensures that everyone must stop and receive clear instructions on where they can go and what biosecurity measures they must follow. Be especially mindful of vehicles that are likely to have traveled to other properties where the infection might be (such as feed store or farm supply delivery trucks or an ambulatory veterinarian’s vehicle which are likely to travel to farmsFor-profit organizations focused on the production and sale of plant and/or animal products.). Whenever possible, have vehicles park in designated areas rather than driving through the property. When this is not possible (such as for fuel delivery trucks), tires and wheel wells should be cleaned and disinfected before they pass through the controlled access point.
Only Allow Essential Staff/Volunteers To Enter Bird Living Spaces
Beyond generally restricting the number of humans and vehicles coming onto your property, also consider if you can further limit the number of humans coming into contact with bird residents. In some situations, this will not be possible, but for sanctuaries with larger teams, perhaps you can have a designated person who cares for the birds (for example having one person care for non-waterfowl bird residents without coming into contact with waterfowl residents). What is necessary and practical will depend on your specific situation and the degree of risk.
Evaluate The Risk Associated With Each Staff Member Or Volunteer
Be sure to consider the potential risk associated with your staff and volunteers and if additional layers of protection should be implemented or if care responsibilities can be adjusted. For example, if one of your volunteers cares for a small flock of chickens in their backyard, they carry a different level of risk than staff members who do not care for birds at home. Perhaps, in order to protect both their companions and your sanctuary’s residents, this staff member could be in charge of caring for mammalian residents only rather than having direct contact with bird residents.
Do Not Share Or Borrow Equipment
In order to prevent bringing the virus to your property, avoid sharing or borrowing equipment. If, for some reason, this is not possible, be sure to consider the risk of virus introduction to your property and ways to mitigate this risk (such as by disinfecting wheels, keeping equipment away from bird areas, etc.)
Create A Protocol To Prevent Humans From Spreading The Virus On Their Clothes, Shoes, or Hands
After limiting the number of humans entering your property and coming into contact with bird residents, be sure to further consider how to reduce the chances those humans could bring the virus in on their clothing, shoes, or hands. This may include asking staff to keep a clean set of clothing and shoes onsite that they change into upon arrival and that are cleaned at the end of their shift. Before entering and upon leaving bird resident living spaces, shoes should either be covered (such as with disposable shoe covers) or cleaned and disinfected with an appropriate footbath solution (more on this below). If it is possible to have a handwashing station outside bird resident living spaces, everyone should wash their hands before and after entry. This may not be feasible in many settings, in which case, disposable gloves should be worn. If you care for multiple flocks, having staff/volunteers wear different clothing or covering their clothing with separate sets of protective gear (such as disposable tyvek suits or long sleeve coveralls) can mitigate the risk of spread between flocks.
A Note About Footbaths
In the past, footbaths have been a common biosecurity measure, but some experts have raised concern that due to the likelihood of incorrect use, foot baths may not be as effective as we need them to be. First, you must use an appropriate solution and concentration (check in with your veterinarian or local officials, as there may be specific solutions you are required to use during times of high HPAI risk). Second, this solution must be changed regularly. Third, in order to work effectively, shoes must be thoroughly cleaned, with all organic material removed, before using the footbath (this can be very difficult in outdoor settings). And lastly, it is imperative that shoes be soaked for an appropriate amount of time (following package or veterinarian instructions). Quickly dipping shoes that are covered in feces and/ or mud into a foot bath is not an effective biosecurity measure.
Keep Resident Spaces And Surrounding Areas Clean, Dry, And Well-Maintained
Cleaning and maintenance are always important aspects of care, but during times when there is high risk of disease spread, they are more important than ever. Cleaning and maintenance measures include:
Daily Cleaning
Be sure to keep resident living spaces clean. If outdoor areas are not fully covered, extra attention should be paid to keep these spaces cleaned so as to remove any sources of infection as soon as possible.
Use Designated Tools Or Disinfect Between Uses
Ideally, separate tools should be used for each flock (keeping in mind that these tools must be stored in an area where they cannot be contaminated). If it is not possible to have separate tools, they will need to be properly disinfected between uses (particularly if they are used in areas wild birds have access to). It may be prudent to use separate tools for resident waterfowl since they are especially susceptible and could be infected without showing obvious signs of illness.
Update November 7, 2024 – Use Separate Tools For Avian And Mammalian Residents
To help protect your avian residents, we recommend using separate tools for your avian and mammalian residents.
Clean And Disinfect Food And Water Containers At Least Once Per Day
In order to further reduce the risk that contaminated food or water could introduce the virus to your residents, be sure to thoroughly clean and disinfect food and water dishes (and store them in a safe space where they cannot become contaminated). Just as with cleaning tools, if you can have designated food and water containers for each flock, that can help prevent disease spread.
Address Drainage Issues
Standing water such as puddles and ponds can attract wild birds and become a source of contamination. Whenever possible, address drainage to prevent these sources of water from forming or cover them to prevent wild birds from accessing them. For larger ponds that cannot be covered, make sure bird residents and anything that comes into contact with them are kept away from these water sources. Of particular concern is the risk of contaminated run-off entering bird resident living spaces.
Keep Parking Areas And Access Roads Clean
In order to reduce the risk of vehicles becoming contaminated and spreading the virus on tires, and to reduce the risk of humans walking through sources of contamination, keep parking areas and access roads as clean as possible. Concrete areas can be more easily kept clean than dirt roads and parking areas, but even these spaces can be regularly cleared of debris.
Make Sure Staff And Volunteers Are Properly Trained And Aware Of Biosecurity Measures
Biosecurity measures are only effective when they are followed consistently and correctly. Whatever measures you have in place, make sure all staff and volunteers are informed and properly trained (this also applies to low-risk times, but is especially important when the risk of infectious disease is high). This includes:
- Making sure staff and volunteers understand the current risk to residents as well as the mechanisms for virus introduction and disease spread and how avian influenza presents
- Thoroughly training all staff on biosecurity protocols and procedures
- Having a written biosecurity plan that is shared with appropriate personnel and updated as needed
- Clearly communicating if/when protocols and procedures change
- Using clear signage to communicate biosecurity measures
Keep Thorough Records
Do not ignore the importance of thorough recordkeeping! In addition to having enhanced biosecurity measures in place, you also want to have a way to prove that these measures are in effect. Be sure to check the regulations in your area as there may be certain records that are mandatory. Otherwise, important records may include:
- A written biosecurity plan including a detailed chain of command and pertinent contact information (in addition to working with your veterinarian to create the plan, you may want to have them sign off on it to demonstrate their involvement)
- Current census information for each living space including the number of residents in each location and their species
- A log of everyone who has had contact with resident birds
- A log of vehicles that have entered sanctuary spaces (name of driver, contact details, dates, times, and purpose of visit)
- Thorough resident records including health history and treatment sheets
- Cleaning logs
- Transport logs* (including trips to the veterinarian)
- Resident movement onsite* (for example if a chicken moves from their flock to your onsite infirmary or into a different flock)
*Keep Resident Movement To A Minimum
During periods of active disease in your region, it’s best to keep resident movement, both onsite and off, to a minimum and to limit it to essential movement only, such as that related to veterinary care. If you care for multiple flocks, restricting movement between flocks (and documenting this information) will help prevent disease spread should one flock become infected.
While creating our chicken care course and discussing notifiable diseases, the veterinarian we worked with stressed the importance of thorough recordkeeping, particularly if you find yourself in a situation where birds in your area are being killed due to a government order to contain an outbreak. We hope no one ever finds themselves in this situation, but we’d urge you to advocate for your residents and to push for an alternative such as maintaining strict quarantine and agreeing to regular testing to prove your residents are not infected. Our reviewing veterinarian stressed that it is much more likely that an exemption would be offered to someone with meticulous written records and individual identification than to someone without.
Intake Considerations
Because new bird residents could introduce avian influenza to your property, putting all of your other bird residents at risk, during times when there are active cases in your region, the question of intake must be carefully considered. While the general response varies region by region and state to state, in the US, a confirmed case in farmed bird species will almost certainly result in the mandated killing of all birds on the property. Unfortunately, even robust quarantine protocols may not be enough to keep everyone safe if you are bringing new bird residents onto your property (or if new birds are being cared for offsite by folks who come onto your property).
In order to continue with active intake while keeping sanctuary residents safe, some organizations have new rescues go directly to approved fosters (who do not already care for birds and who do not work or volunteer onsite at the sanctuary). By keeping new residents offsite and away from the sanctuary’s onsite staff and volunteers, sanctuary residents should be safe in the event that the new resident has been exposed to HPAI. Other organizations have required that any new avain residents be tested for avian influenza before being allowed on the property. If you are considering implementing testing of new rescues before they come into contact with your staff or set foot on your property, we recommend you have a conversation with your veterinarian about if and how you should go about this. If neither of these options are available, unfortunately, suspending intake is the only way to ensure that a new avian resident cannot introduce the virus to your property. Because the degree of risk varies based on where you are located, we recommend having a conversation with a trusted veterinarian about your specific situation and best course of action.
Update November 7, 2024 – Intake Of Mammalian Residents May Put Your Bird Residents At Risk
The recent detections in mammalian farmed animal species indicate that we now have to also consider the possibility of newly rescued mammalian residents bringing HPAI onto sanctuary grounds, though current evidence suggests that lactating cows pose the biggest risk. In addition to the risk of the virus being spread to your avian residents and causing serious illness or the virus being spread to humans at the sanctuary, we simply don’t know what a positive detection in a mammalian sanctuary resident would mean for avian residents on the property (in terms of government response).
ACTION STEPS TO PROTECT YOUR RESIDENTS FROM HPAI:
1. Regularly monitor conditions in your area by checking with your veterinarian and local authorities to stay apprised of new information and risks.
2. Enforce your existing biosecurity protocols and assess what additional protective measures you can implement to enhance your residents’ safety. These measures may include but are not limited to:
- Using carefully maintained footbaths in conjunction with veterinary guidance;
- Using PPE such as foot coverings and disposable gloves;
- Securing sanctuary tools and equipment in such a way as to protect them from contact with wildlife;
- Limiting access to sanctuary grounds by personnel and vehicles which may have had exposure;
- And providing caregivers with safe space to change clothing before and after contact with residents.
3. Evaluate your existing infrastructure and consider modifications that can protect residents, such as:
- Adding solid roofing or dense netting to living spaces and runs;
- Taking measures to make sure that all wildlife is excluded from resident living spaces;
- Ensuring that wildlife cannot access resident food supplies or any tools used in maintaining resident living space;
- Considering how access to sanctuary features such as ponds can be restricted either from wildlife access, or from sanctuary residents;
- Safeguarding resident living spaces from runoff from water that may have been accessed by wildlife;
- And creating boundaries with respect to access by outside vehicles that may have been in areas where the virus has been found
4. Consider your existing administrative framework for dealing with documentation around biosecurity, medical monitoring of residents, and documentation of veterinary care, as well as your written plans with respect to all of these.
- Consult with your vet to develop a plan well in advance of an outbreak in your area.
- And document your biosecurity measures and any changes you make in response to changing risks in your area, including maintaining daily logs concerning: caregivers of residents; logs of vehicles entering sanctuary spaces; logs with respect to resident health status and treatments; cleaning logs; and transport logs.
Resource Acknowledgments
We extend our deepest gratitude to the folks at Brockswood Animal Sanctuary and to Elaine Maltezos, of Bergen Chicken Sanctuary, for sharing their own experiences responding to HPAI outbreaks and regional control efforts. We continue to welcome additional input and experience from the sanctuary world.
SOURCES:
What Are The Different Types Of Avian Influenza? | USGS
Diseases Of Poultry 13th Edition | David E. Swayne (Non-Compassionate Source)
Avian Influenza | World Health Organisation For Animal Health (OIE) (Non-Compassionate Source)
Avian Influenza | Merck Veterinary Manual (Non-Compassionate Source)
Avian Influenza In Birds | Centers For Disease Control And Prevention (Non-Compassionate Source)
Declaration of Avian Influenza Prevention Zone – Including Housing Measures (England) | Department For Environment, Food and Rural Affairs (Non-Compassionate Source)
Biosecurity And Preventing Welfare Impacts In Poultry And Captive Birds | Department For Environment, Food, And Rural Affairs (Non-Compassionate Source)
Avian Influenza In The Forecast: Are You Ready? | USDA APHIS (Non-Compassionate Source)
Defend The Flock: Preventing Avian Influenza Introductions: Focus On The Big Risks | USDA APHIS (Non-Compassionate Source)
What Does It Mean For You Who Have Hens In The Garden If Bird Flu Is Detected In The Immediate Area? | Mattilsynet (Norwegian Food Safety Authority) (Non-Compassionate Source)
About The Gate Prohibition Regulations For Poultry | Mattilsynet (Norwegian Food Safety Authority) (Non-Compassionate Source)
2022 Highly Pathogenic Avian Influenza | USDA APHIS(Non-Compassionate Source)
Avian Influenza Viruses Can Persist In Footbaths And Manure | Poultry Health Today (Non-Compassionate Source)
Update On HPAI Detection In Wild Bird | USDA APHIS (Non-Compassionate Source)
Antimicrobial Products Registered for Disinfection Use Against Avian Influenza on Poultry Farms and Other Facilities | United States Environmental Protection Agency (Non-Compassionate Source)
Wild Bird Highly Pathogenic Avian Influenza Surveillance | Food And Agriculture Organization Of The United Nations (Non-Compassionate Source)
Non-Compassionate Source?
If a source includes the (Non-Compassionate Source) tag, it means that we do not endorse that particular source’s views about animals, even if some of their insights are valuable from a care perspective. See a more detailed explanation here.