
Veterinary Review Initiative
This resource has been reviewed for accuracy and clarity by a qualified Doctor of Veterinary Medicine with farmed animal sanctuaryAn animal sanctuary that primarily cares for rescued animals that were farmed by humans. experience as of January 2023.
Check out more information on our Veterinary Review Initiative here!
Unfortunately, as much as we wish it weren’t the case, taking on the lifelong care of another living being means that, at some point, you will likely have to care for them through periods of illness. When our residents are sick, we hope that these periods of illness will be brief and mild. When dealing with issues that are treatable, we make sure we can get them the medicine they need to recover. But what happens when treatments that should work, don’t? While there could be a variety of reasons for an individual not responding to treatment, one important issue caregivers should be aware of is drug resistance. In this resource we are going to take a closer look at antimicrobial and anthelmintic resistance and what sanctuaries can do to slow the development of resistance in these types of drugs.
Antimicrobial Resistance
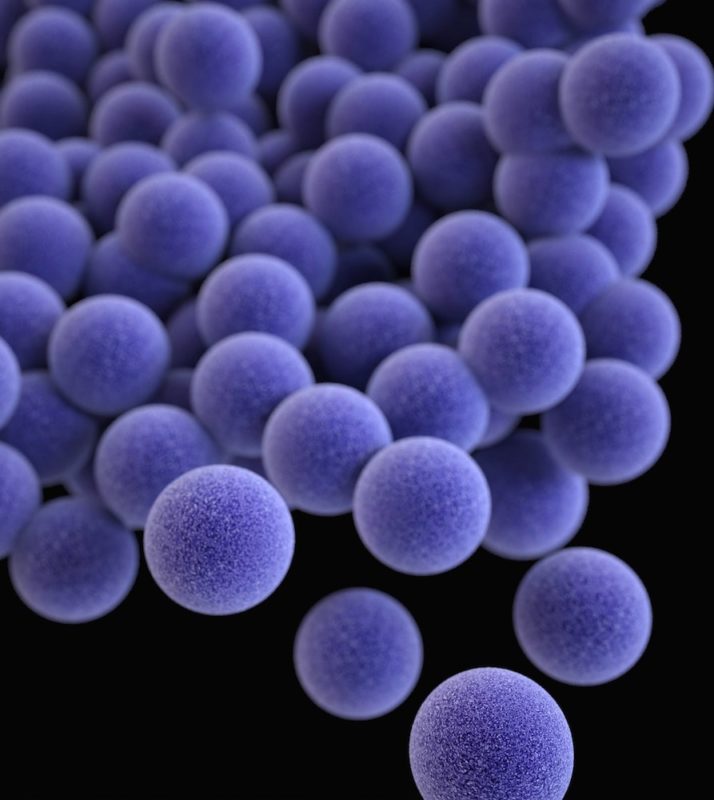
Antimicrobial resistance is a serious problem that can make it difficult or impossible to treat certain types of infection.
What Are Antimicrobials?
Antimicrobials are products that kill or slow the growth of microorganisms (microscopic organisms). They can be categorized by the type of microorganism they work against and include antibiotics (used for bacterial infections), antivirals (used for viral infections), antifungals (used for fungal infections), and antiprotozoals (used for protozoan infections). Antimicrobials play a crucial role in both veterinary and human medicine (however, antivirals are not as commonly used in veterinary medicine).
What Is Antimicrobial Resistance?
Antimicrobial resistance does not mean the individual being treated has developed resistance to a drug, it means the microorganism they are infected with has developed resistance. Antimicrobial resistance occurs when microorganisms change over time and develop the ability to withstand antimicrobial treatment. As mentioned above, antimicrobials work by killing or slowing the growth of microorganisms. When microorganisms develop resistance, they are able to survive or continue to reproduce despite antimicrobial treatment. This can make it difficult or even impossible to treat certain infections.
When talking about the issue of antimicrobial resistance, the focus is not on microorganisms that have always been resistant to a particular drug. Instead, the focus is on acquired resistance: microorganisms that were at one point susceptible to a particular antimicrobial but have developed the ability to withstand the treatment. Some microorganisms are now resistant to multiple antimicrobials. A commonly known example is methicillin-resistant Staphylococcus aureus (MRSA). MRSA has been reported in numerous farmed animalA species or specific breed of animal that is raised by humans for the use of their bodies or what comes from their bodies. species, including horses, pigs, and chickens and has the potential for zoonotic transmission (transmission to humans).
Is Antimicrobial Resistance The Same Thing As Antibiotic Resistance?
The short answer is no. Antimicrobial resistance includes antibiotic resistance, but also applies to other types of microorganisms besides just bacteria. To better understand the difference between antimicrobial resistance and antibiotic resistance, let’s start by considering the difference between antibiotics and antimicrobials. Antibiotics are just one type of antimicrobial – so while all antibiotics are also antimicrobials, not all antimicrobials are antibiotics. For example, an antifungal is also an antimicrobial, but it is not an antibiotic.
To use examples that may be more familiar to sanctuary folks, consider that a specific breed of animal is just one of many breeds: all Cornish crosses are chickens, but not all chickens are Cornish crosses. Similarly, a particular species is just one example of a broader group of animals: all sheep are ruminants, but not all ruminants are sheep. The same is true for antibiotics and antimicrobials – antibiotics are one specific type of antimicrobial. The term antimicrobial encompasses more than just antibiotics, and antimicrobial resistance encompasses more than just antibiotic resistance.
However, confusion between the two is understandable. Over the years, there has been a significant focus on antibiotic resistance, so for some folks, the concept of “antibiotic resistance” may be much more familiar than the broader concept of “antimicrobial resistance.” In recent years, there has been a push for more awareness of antimicrobial resistance. As such, in 2020, the global campaign formerly known as “World Antibiotic Awareness Week” was renamed “World Antimicrobial Awareness Week” so as to include other antimicrobials.
Another reason antimicrobial resistance and antibiotic resistance are sometimes used interchangeably may be due to the fact that antibiotics are often the most frequently used antimicrobials in sanctuary spaces. Additionally, it is not at all uncommon for sanctuary residents to develop (or arrive with) antibiotic-resistant bacterial infections. To learn more about antimicrobial-resistant pathogens (specifically, drug-resistant bacteria) that are a concern in the US, check out this report from the American Veterinary Medical Association (AVMA).
What Causes Antimicrobial Resistance?
According to The National Institute Of Allergy And Infectious Diseases, “Microbes, such as bacteria, viruses, fungi, and parasites, are living organisms that evolve over time. Their primary function is to reproduce, thrive, and spread quickly and efficiently. Therefore, microbes adapt to their environments and change in ways that ensure their survival. If something stops their ability to grow, such as an antimicrobial, genetic changes can occur that enable the microbe to survive.” This process occurs naturally over time. However, certain practices can accelerate this process. The World Health Organization lists the misuse and overuse of antimicrobials as one of the major drivers of accelerating rates of antimicrobial resistance. The use of antibiotic feeds in animal agricultureThe human production and use of animals in order to produce animal products, typically for profit. may be significantly contributing to antimicrobial resistance.
You Can Help Slow Antimicrobial Resistance Outside Of Sanctuary Spaces, Too!
The issue of antimicrobial resistance goes beyond the use of antimicrobials in non-human animals. When it comes to human medicine, non-medical professionals sometimes view antibiotics as the answer for just about everything. But just as antibiotics aren’t always the answer when one of our residents is sick, the same is true when we’re sick. Instead of asking for antibiotics any time you (or a human you care for) isn’t feeling well, talk with your doctor about what they suspect the problem to be and whether or not antibiotics are recommended. Even if the issue is a bacterial infection, treatment may not be necessary.
How Does Antimicrobial Resistance Affect Sanctuaries?
Unfortunately, antimicrobial resistance can develop at animal sanctuaries just like anywhere else. It’s also possible for a new resident to bring a drug-resistant microorganism into sanctuary spaces. As mentioned above, antimicrobial resistance can make it difficult or even impossible to treat infection. Because of their designation as “food animals,” farmed animal species already tend to have limited options when it comes to antimicrobial treatment, and antimicrobial resistance further limits the available options. Once the available treatment options are exhausted, caregivers are left in the awful position of having no way to treat the individual’s infection. This may have an immediate and devastating impact on the individual’s quality of life, depending on the infection they are dealing with.
Not only does antimicrobial resistance affect individual(s) who have drug-resistant infections, it can also put other residents at risk of becoming infected with the same difficult or impossible to treat infection. Measures that are necessary to protect other residents from infection could have a negative impact on the quality of life of the infected individual (if strict isolationIn medical and health-related circumstances, isolation represents the act or policy of separating an individual with a contagious health condition from other residents in order to prevent the spread of disease. In non-medical circumstances, isolation represents the act of preventing an individual from being near their companions due to forced separation. Forcibly isolating an individual to live alone and apart from their companions can result in boredom, loneliness, anxiety, and distress. is necessary) or on the other residents (such as if a resident must be separated from their close companion). In the case of a zoonotic infection (one that can spread to humans), humans who come into contact with residents are also at risk. If zoonotic diseaseAny disease or illness that can be spread between nonhuman animals and humans. impacts staff, volunteers, or guests, your organization may also face potential liability.
In addition to the direct impacts of antimicrobial resistance, sanctuaries are also affected by the measures put into place to slow the development of antimicrobial resistant infections in humans. For example, in 2015, the Food And Drug Administration (FDA) banned the use of enrofloxacin (“Baytril”) in “poultry” due to concerns about resistance in Campylobacter jejuni. At the time of the decision, the AVMA issued a statement saying the association was “concerned that the withdrawal of the drug will negatively impact poultry health and welfare. The alternatives to enrofloxacin are few in number and less effective.” This ban leaves veterinarians with one less option when treating certain bacterial infections in chickens, turkeysUnless explicitly mentioned, we are referring to domesticated turkey breeds, not wild turkeys, who may have unique needs not covered by this resource., ducksUnless explicitly mentioned, we are referring to domesticated duck breeds, not wild ducks, who may have unique needs not covered by this resource., geeseUnless explicitly mentioned, we are referring to domesticated goose breeds, not wild geese, who may have unique needs not covered by this resource., and other avian species designated as “food animals” or “food producing animals.”
Unlike some in other settings, where humans may seek out the healthiest animals or only buy animals that have been confirmed to be free of certain diseases, farmed animal sanctuariesAnimal sanctuaries that primarily care for rescued animals that were farmed by humans. typically rescue those most in need. As a result, sanctuaries often take in residents who have come from situations where they were under extreme stress and were potentially exposed to infectious disease. The individuals may be in very poor health and may require antimicrobial treatment in order to save their life. Additionally, due to the ways in which farmed animalsA species or specific breed of animal that is raised by humans for the use of their bodies or what comes from their bodies. have been bred, some species are prone to chronic health conditions that may require antimicrobial treatment or which may put them at risk of developing infections that will require treatment. Between rescuing sick individuals and caring for individuals suffering from the impacts of domestication, maintaining the health and well-being of sanctuary residents often depends on the appropriate use of antimicrobials. When the available list of antimicrobials shrinks, either due to the development of resistant infections or because of the banning of certain treatments, our ability to care for these individuals is negatively impacted.
Anthelmintic Resistance
While perhaps not technically antimicrobial resistance, we’d be remiss if we talked about drug resistance without mentioning anthelmintic resistance, a growing issue worldwide.
What Are Anthelmintics And What Is Anthelmintic Resistance?
Anthelmintics, or dewormers, are drugs that kill or remove helminths (parasitic worms), such as nematodes (roundworms), cestodes (tapeworms), and trematodes (flukes). Just as microorganisms develop resistance to antimicrobials naturally over time, helminths develop resistance to anthelmintics.
What Causes Anthelmintic Resistance?
As with antimicrobial resistance, anthelmintic resistance is a natural evolutionary process. And just as the overuse and misuse of antimicrobials can accelerate the rate at which resistance to antimicrobials develops, so too does the overuse and misuse of anthelmintics accelerate the rate at which helminths develop resistance to dewormers. However, Dr. Kaplan, Professor of Veterinary Parasitology at University of Georgia, explains that parasitic worms have certain characteristics that “favor the development of drug resistance.” These include short life cycles, high reproductive rates, high rates of genetic mutation, and very large population sizes.
Through random genetic mutation, there will always be some worms within a species that are not susceptible to a certain drug, without ever having been exposed to the drug before. However, these mutations are rare and occur in very low numbers compared to the rest of the worm population that does not have this mutation and is susceptible. When a worm population is exposed to a dewormer, worms with a mutation that allows them to withstand the treatment will have an advantage, while those without the mutation will be killed. Every time this occurs, the ratio of resistant-to-susceptible parasites increases, resulting in an increased chance of two resistant worms mating with each other and passing along this drug resistance to the next generation of worms. Unfortunately, without using diagnostic tools to assess whether or not resistance is an issue at your sanctuary, this growing issue can go undetected until you have an irreversible problem on your hands.
How Does Anthelmintic Resistance Affect Sanctuaries?
Anthelmintic resistance can develop at sanctuaries over time, and new residents may arrive harboring anthelmintic-resistant parasites. As with antimicrobial resistance, when sanctuaries are dealing with anthelmintic resistance, they risk finding themselves in a situation where a resident (or multiple residents) have parasitic infections that are difficult or impossible to treat. Dewormers are a limited resource and, typically, resistance to one drug in a particular class of drugs results in resistance to all drugs in that class. Haemonchus contortus, a dangerous blood-sucking gastrointestinal roundworm of small ruminants and camelids, is perhaps the most well-known example of anthelmintic resistance and is a significant concern for sanctuaries in many areas. If you care for sheep, goats, llamas, or alpacas, this is an issue you should be aware of – you can find our in-depth resource on the subject here. Anthelmintic resistance has also been documented in other species, as well, including horses, cowsWhile "cows" can be defined to refer exclusively to female cattle, at The Open Sanctuary Project we refer to domesticated cattle of all ages and sexes as "cows.", pigs, and turkeys.
Even though anthelmintics may be available without a prescription, it is imperative that they be used appropriately. We strongly recommend that sanctuaries work closely with an experienced veterinarian to develop strategies to prevent these infections (when possible), and to create protocols to screen residents for infection. DewormingThe act of medicating an animal to reduce or eliminate internal parasites, either prophylactically or in response to illness. decisions should be made with your veterinarian to ensure that individuals who require treatment are treated appropriately while also avoiding administering treatment unnecessarily. Additionally, treatment efficacy should be monitored to watch for signs of growing resistance. Deworming is often a nuanced decision that needs to be made on a case-by-case basis.
What Can Sanctuaries Do To Slow The Rate Of Antimicrobial And Anthelmintic Resistance?
The issue of antimicrobial and anthelmintic resistance extends far beyond the sanctuary world, but that doesn’t mean there isn’t anything sanctuaries can do! Enacting certain practices can help keep your residents safe and slow the development of both antimicrobial and anthelmintic resistance. We recommend having a discussion (or many!) with your veterinarian to determine specific strategies for your sanctuary, particularly when creating a parasite management strategy. In the meantime, here’s a list to get you started:
- Focus on prevention. You can reduce the need for antimicrobials and anthelmintics by implementing practices that prevent infection in the first place. In some cases, this is more easily said than done, and how exactly you do this will depend on the infections your residents are most vulnerable to, but might include the following:
- Enact or enhance biosecurity practices
- Improve sanitation practices
- Implement fly mitigation practices and address other disease vectors such as ticks, lice, rodents or other wildlife, etc.
- Reduce or eliminate your residents’ exposure to harmful microorganisms and helminths in their environment, which may mean implementing careful pasture rotation for grazing residents, keeping wild animals out of resident spaces as much as possible, avoiding certain bedding options, and/or restricting your residents’ access to areas that are more likely to expose them to certain diseases (such as restricting access to wet areas during certain times of year)
- Follow strict quarantine procedures for incoming residents and perform diagnostics to screen for infection (as recommended by your veterinarian)
- Implement isolation protocols when infectious disease is suspected
- Establish a vaccination protocol for residents, in consultation with your veterinarian
- Implant chickens and other bird residents when possible and appropriate
- Focus on overall resident health. Preventing exposure to harmful organisms is important, but it is just part of the equation. Individuals who are malnourished or constantly under stress are much more vulnerable to disease. Luckily, the reverse is also true! Healthy residents who are not constantly under stress are often better able to ward off illness. They may be less likely to become infected in the first place, or they may be less likely to develop clinical disease that requires treatment with antimicrobials or anthelmintics. To promote optimal resident health, you should:
- Assess resident nutrition to ensure everyone is fed an appropriate diet that meets their nutritional needs and promotes good health
- Ensure residents have access to clean, palatable drinking water
- Evaluate resident housing and make changes as needed to promote healthy air quality and to prevent temperature related stress (ex. improved ventilation, maintaining a suitable indoor temperature, avoiding extreme temperature fluctuations, etc.)
- Find ways to reduce resident stress levels by offering ample space and resources, creating healthy social groupings (making changes when necessary), and helping to make unavoidable situations that tend to cause stress (ex. transport to the vet or health treatments) neutral or even positive by taking time to provide compassionate learning opportunities for residents.
- Ensure antimicrobials and anthelmintics are used correctly and appropriately. Even with the best preventative measures, there will inevitably be times when antimicrobials or anthelmintics are necessary in order to ensure the health and well-being of the individual. The goal of the above strategies is to reduce the need for antimicrobial and anthelmintic use – it is not to avoid use of these treatments entirely. To prevent overusing and misusing antimicrobials and anthelmintics, you should:
- Consult with an experienced veterinarian about all antimicrobial and anthelmintic treatments even if you don’t need a prescription to secure the medication
- Request diagnostics (culture and sensitivity, fecal testing, etc.), when possible, to ensure the most appropriate treatment is implemented
- Follow your veterinarian’s instructions (or label instructions) to ensure proper dose, frequency, duration, administration route, etc. (and make sure anyone administering the treatment is properly trained – improper administration could result in underdosing, among other things)
- Use current resident weights, whenever possible (rather than estimating their weight or using an old weight), in order to ensure proper dosing
- Check in with your veterinarian about the individual’s progress on treatment so that they can re-evaluate and/or perform follow-up diagnostics as needed
- When using anthelmintics, perform post-treatment diagnostics, when possible, to assess whether or not the treatment was effective and to determine if resistance appears to be an issue
Follow Storage Instructions And Adhere To Expiration Dates!
Not observing storage recommendations can reduce the efficacy of drugs and contribute to resistance. Similarly, using drugs past their expiration date can also result in using medication that is less effective. While there is some debate about the validity of current expiration dates for certain drugs, particularly those in solid form like pills and capsules, we strongly recommend
that you check in with your veterinarian or pharmacist before using expired medications. They can advise you based on the medication in question and stamped expiration date.
Finding The Right Veterinarian Is Imperative!
Because the species farmed animal sanctuaries care for are typically viewed by society at large as commodities, finding compassionate individualized veterinary care can be a challenge. We’ve certainly heard of veterinarians defaulting to euthanasia over treatment, sometimes to the point of refusing to prescribe antibiotics or other treatments, even if there is reason to believe that the treatment is reasonable. It’s understandable that folks who have experienced this firsthand or who have heard these horror stories might be skeptical about relying on veterinarians for all treatment decisions and may, instead, be inclined to reach for a bottle of leftover antibiotics “that worked last time” or that worked for another resident. While we certainly understand where this inclination may come from, ultimately, veterinarians are the only trained professionals who can make recommendations about antimicrobial use, and when it comes to antibiotics, in many cases a prescription is required (by June 2023, all “medically important antibiotics” will require a prescription in the US). While anthelmintics are easy to secure without veterinary involvement, the right veterinarian can play an integral role in ensuring their proper use and in recognizing and responding to signs of anthelmintic resistance.
While it can sometimes take time to find the right veterinarian, there are amazing veterinarians out there who are invested in providing the compassionate individualized care sanctuaries expect for their residents. Depending on a veterinarian’s background and experience, there may be times when you have treatment ideas that they wouldn’t have thought of on their own, and there may be times when you have more experience with a certain disease than they do. The “right” veterinarian won’t necessarily have all the answers, but they should be open to having discussions about treatment options and be willing to answer your questions about why a treatment may or may not be appropriate. If necessary, they can also consult with other veterinarians to determine if the treatment you suggest is appropriate in this particular instance.
Addressing the issues of antimicrobial and anthelmintic resistance requires that everyone who uses these drugs does so responsibly. Therefore, while resistance issues are not unique to sanctuaries, and the use of these medications in sanctuary settings may not contribute to resistance to the same degree (or at the same rate) as their use in large scale agricultural operations, it is still important that sanctuaries do their part to address this growing issue.
In sanctuary spaces, we use these treatments because of our commitment to resident health and well-being. If someone is sick, we want to help them. If we’re worried someone has been exposed to harmful organisms or has an infection that might make them sick, we want to address the issue before it becomes a more serious problem. This commitment to the individuals in our care is a fundamental aspect of providing sanctuary. However, it’s important to recognize that overusing and misusing antimicrobials and anthelmintics can ultimately cause more harmThe infliction of mental, emotional, and/or physical pain, suffering, or loss. Harm can occur intentionally or unintentionally and directly or indirectly. Someone can intentionally cause direct harm (e.g., punitively cutting a sheep's skin while shearing them) or unintentionally cause direct harm (e.g., your hand slips while shearing a sheep, causing an accidental wound on their skin). Likewise, someone can intentionally cause indirect harm (e.g., selling socks made from a sanctuary resident's wool and encouraging folks who purchase them to buy more products made from the wool of farmed sheep) or unintentionally cause indirect harm (e.g., selling socks made from a sanctuary resident's wool, which inadvertently perpetuates the idea that it is ok to commodify sheep for their wool). than good. Therefore, it is imperative that caregivers familiarize themselves with the issues of antimicrobial resistance and anthelmintic resistance and that they enact protocols to protect residents from infection as much as possible. When antimicrobial or anthelmintic use is necessary, caregivers should work closely with an experienced veterinarian to determine the most appropriate treatment and then follow their instructions to ensure proper dose and administration.
Infographic
Looking to share information about antimicrobial resistance in an accessible way? Check out and share our infographic below!
Top Section/Section 1
Image on left: Pill bottles, blister pack, and capsules
Text on left under image: Antimicrobials are products that kill or slow the growth of microorganisms like bacteria, viruses, fungi, and protozoans and includes antibiotics.
Image on right: 3 red germs behind a fourth germ that is brighter red and has an evil face
Text on right under image: Resistance occurs when microorganisms change over time and develop the ability to withstand antimicrobial treatment.
Section 2 (under section 1)
Text: “Microbes adapt to their environments and change in ways that ensure their survival. If something stops their ability to grow, such as an antimicrobial, genetic changes can occur that enable the microbe to survive.” – The National Institute Of Allergy And Infectious Diseases
Section 3 (under section 2)
Text: Resistance develops naturally over time, but the misuse and overuse of antimicrobials is one of the major drivers of accelerating rates of resistance. To reduce the need for antimicrobial use…
Column on left – heading: Focus On Prevention
Subheading on left: Implement practices that prevent infection.
Bullet points on left:
– BiosecurityMerck Veterinary Manual defines biosecurity as ”the implementation of measures that reduce the risk of the introduction and spread of disease agents [pathogens].” measures
– QuarantineThe policy or space in which an individual is separately housed away from others as a preventative measure to protect other residents from potentially contagious health conditions, such as in the case of new residents or residents who may have been exposed to certain diseases. + isolation
– Vaccination programs
– Fly mitigation
– And more!
Image on left: cartoon drug vial holding a shield and syringe
Column on right – heading: Promote Health
Subheading on right: Healthy residents are often better able to ward off illness.
Bullet points on right:
– Healthy, nutritious diets
– Clean, palatable water
– Proper ventilation
– Healthy group dynamics
– And more!
Bottom Section/Section 4
Text: Even with the best preventative measures, there will be times when antimicrobials are necessary. To ensure antimicrobials are used correctly and appropriately…
Bullet points:
– Consult with a veterinarian about all antimicrobial use
– Request diagnostics, when possible
– Follow instructions regarding dose, frequency, duration, etc.
– Use actual and current weights for calculating drug dosages
– Check in with your vet about the individual’s progress on treatment
Images: A written prescription (top right corner of section); a veterinarian in white coat and mask writes on a clipboard (bottom right corner of section); three pill bottles, with “rx” written on the front bottle (bottom left corner of section)
Text at bottom of infographic: Learn more at opensanctuary.org
SOURCES:
Causes Of Antimicrobial (Drug) Resistance | National Institute Of Allergy And Infectious Diseases
Antimicrobial Use And Antimicrobial Resistance | AVMA
Antimicrobial Resistance | World Health Organization
World Antimicrobial Awareness Week | World Health Organization
FDA Stops The Use Of Enrofloxacin For Bacterial Infections In Poultry | AVMA
Be Antibiotics Aware Partner Toolkit | Centers For Disease Control And Prevention
Methicillin-Resistant Staphylococcus aureus | Iowa State University
Advanced Topics In Resident Health: Barber Pole Worm | The Open Sanctuary Project
Anthelmintic Resistance In Equine Nematodes | Jacqueline B. Matthews
Drug Expiration Dates — Do They Mean Anything? | Harvard Health Publishing
Antimicrobial Resistant Pathogens Affecting Animal Health In The United States | AVMA/Committee On Antimicrobials (Non-Compassionate Source)
How And Why Resistance To Worm Remedies Develops | Dr. Ray M. Kaplan( Non-Compassionate Source)
Resistance To Anthelmintics | Merck Veterinary Manual (Non-Compassionate Source)
Anthelmintic Resistance In Cattle Nematodes In The US | Louis C. Gasbarre (Non-Compassionate Source)
The Impact Of Anthelmintic Resistance In Parasites Of Poultry | Zootecnica International (Non-Compassionate Source)
Non-Compassionate Source?
If a source includes the (Non-Compassionate Source) tag, it means that we do not endorse that particular source’s views about animals, even if some of their insights are valuable from a care perspective. See a more detailed explanation here.